Varicose Veins
Home » Varicose Veins
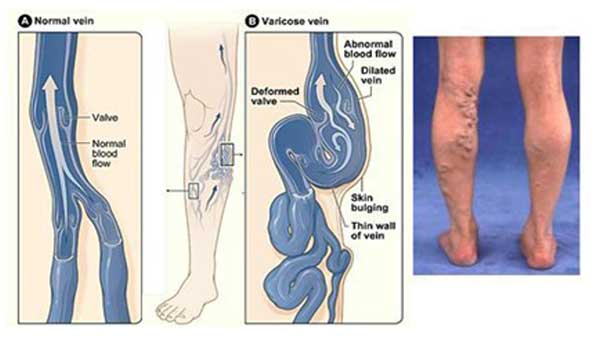
Description of Varicose Veins
Varicose veins are abnormally dilated, visible, tortuous veins in your legs which are caused by incompetent venous valves in your legs. This incompetency leads to engorged veins with high venous pressure which can cause aching, heaviness, throbbing and leg cramps. If left untreated a minor proportion of patients with varicose veins can get complications of thrombophlebitis, bleeding, skin eczema, leg swelling and venous ulcers. The actual underlying cause of primary varicose veins is not known however few predisposing factors include prolonged standing, tall stature, age, obesity, female gender, lack of exercise and family history. Varicose veins can also develop secondary to Deep Venous Thrombosis (DVT), trauma to deep veins or venous obstruction from any cause.
Investigation
Varicose veins are a clinical diagnosis. A Venous Duplex scan is mandatory before any intervention. It is an ultrasound scan of the veins which identifies the exact sites of incompetence that helps your surgeon choose the best possible treat- ment for your veins. It also examines the deep veins which is the major venous drainage for the legs. Interventions for vari- cose veins are generally contraindicated if you have deep venous incompetence as the varicose veins act as collateral drain- age in this situation. Your doctor will be able to prescribe a suitable pair of venous stockings which must be worn lifelong for deep venous incompetence.
Treatment Options for Varicose Veins
There are a variety of treatment options available, each with its own pros and cons. Dr Bhutia is able to discuss these with you and suggest the best possible option (s) for you.
Open Surgery
Open surgery is a time-tested option and still considered one of the most effective treatment options for varicose veins. The operation takes about one hour and is performed as a day case procedure, under general anaesthesia. It usually involves a cut in the groin or in the back of the knee (depending on the scan findings). The incompetent venous system is tied off, disconnected from the rest of the system and stripped out. Multiple small stab incisions are then made over the varicose veins and the veins removed.
Pros: Time-tested, durable, veins are physically removed from the body. Low recurrence rates.
Cons: Higher rates of surgical wound-related complications including wound infection, hematoma formation, nerve injuries and scarring. The return to normal activities is usually 7-10 days without complications.
Radio Frequency Ablation
Pros: minimally invasive procedure, avoids a cut in the groin/back of the knee and the consequent potential wound-related complications. Return to normal activities is quicker in about 3 days.
Cons: The heat energy can cause minor skin burns. The treated segment of vein will generate mild phlebitis which is short lived but rarely be prolonged causing pain for 1-2 weeks.
Endovenous Laser
It is similar to RFA except that a LASER fibre is used instead of a RFA catheter and the vein is treated using heat generat- ed by LASER. This is not currently available in Cairns Private Hospital.
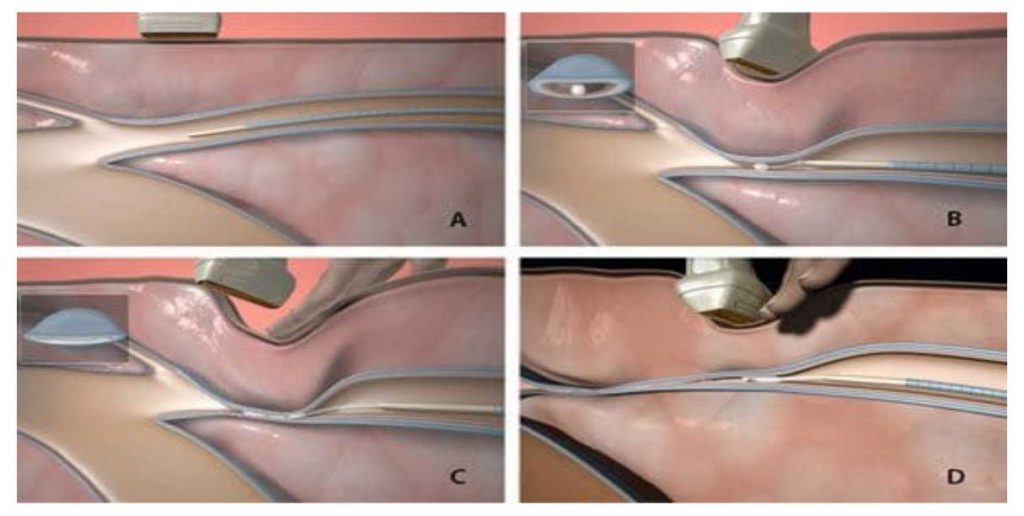
Endovenous Glue Ablation (Venaseal)
The Venaseal procedure is an endovenous procedure whereby a catheter is inserted into the vein using ultrasound guid- ance. Through the catheter small amounts of medical glue is delivered into the vein under ultrasound guidance to seal the vein. The treated vein is left in situ for the body to absorb it away. Multiple small stab incisions are then made over the varicose veins and the veins removed. Dr Bhutia is an early adopter of this procedure in Australia and performs the proce- dure under general anaesthesia as a day case.
Pros: Minimally invasive treatment, no surgical cut involved, excellent early and mid-term results. Minimal pain and no need for compression bandage/stockings afterwards.
Cons: The glued segment of vein can leave a fine brown pigmented line in light-skinned individuals. The medical glue can elicit an allergic reaction in 1:10000. It is not very effective for large superficial veins. Long-term results are not known as it is a relatively new technique.
Micro Sclerotherapy
Micro sclerotherapy involves the injection of a sclerosing solution into veins using a fine needle which causes the venous wall to shut down. This technique is used to treat thread veins/spider veins for cosmetic improvements. The treated vein is kept compressed with a compression bandage for the first 2 days and with a compression stocking over the next 2 weeks. Optimal results may take up to 3 months and it may require several session of injection treatment to the affected area.
Foam Sclerotherapy
Foam Sclerotherapy involves the injection of a sclerosing solution mixed with air to create a fine foam particle. The foam induces shutdown of the venous wall and thrombosis. The foam is easily visible under ultrasound which is used to guide the treatment. The treated vein is kept compressed with a compression bandage for the first 2 days and with a compression stocking over the next 4 weeks. This is an effective treatment for any residual veins left over after an open surgery/rfa/glue treatment or for recurrent veins. Optimal results may take up to 3 months and it may require several sessions of injec- tion treatments to the affected area.
Side effects from sclerotherapy are usually mild, including minor rash-like reaction, and fine brown skin staining, and re- solve themselves quickly.